Hope for diabetes: CRISPR-edited cells pump out insulin in a person – and evade immune detection

Edits create cells that don’t trigger an immune response, allowing implant recipient to forego immune-suppressing drugs
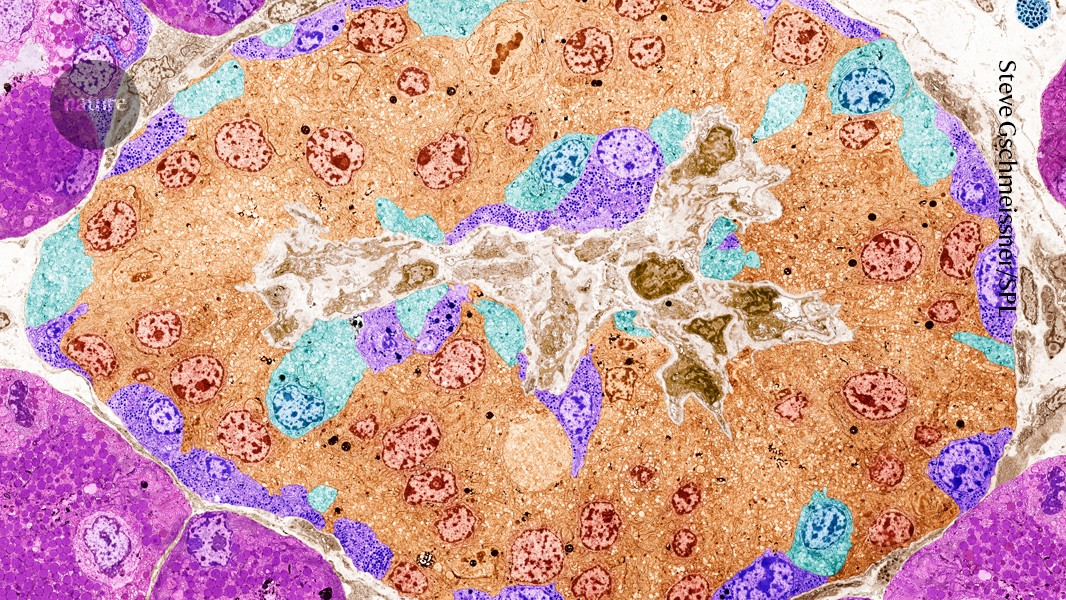
Pancreatic islets (artificially coloured) no longer secrete sufficient insulin in people with type 1 diabetes. Credit: Steve Gschmeissner/Science Photo Library
In a medical first, researchers report that they have implanted CRISPR-edited pancreas cells into a person with type 1 diabetes. The cells pumped out sugar-regulating insulin for months — without the need for the recipient to take immune-dampening drugs, thanks to gene edits that allowed the cells, collected from a deceased donor, to evade detection by the recipient’s immune system1.
The study, orchestrated by the firm Sana Biotechnology in Seattle, Washington, raises hopes of an enduring cure for an autoimmune disease that consigns millions of people to a life of strict monitoring and dependence on injected insulin. “The preliminary data has definitely lifted the spirits of our community — and it’s a really elegant approach”, says Aaron Kowalski, the chief executive of Breakthrough T1D, a non-profit organization in New York City formerly known as JDRF.
The ultimate goal is to apply immune-cloaking gene edits to stem cells and then direct their development into insulin-secreting islet cells. Unedited islets made from stem cells have already shown promise for treating type 1 diabetes in a small trial, according to results published in June2.
But some independent research groups have failed to confirm that the Sana method confers immune-skirting abilities on edited cells. And the study involved only one person who received a low dose of cells for a short time — not enough “to achieve insulin independence, so clinical efficacy remains unproven”, says Tim Kieffer, a molecular endocrinologist at the University of British Columbia in Vancouver, Canada.
Still, Kieffer calls the demonstration of immune cloaking “convincing” and “a major milestone toward the goal of effective cell therapy without chronic immunosuppression”. Kieffer previously held the role of chief scientific officer at biotechnology company ViaCyte (that has since been acquired by Vertex Pharmaceuticals in Boston, Massachusetts), which, like Sana, focused on developing cell therapies for type 1 diabetes.
Stem-cell solutions
Currently, the only way for someone with type type 1 diabetes to avoid dependence on injected insulin is through the transplantation of cadaveric islet cells. The procedure can restore insulin production for years, but it is rarely performed — constrained by the scarcity of donor pancreases and the need for lifelong immune-suppressing drug therapy, which carries risks of infection, cancer and other serious side effects.
To address the donor shortage, some companies have turned to stem-cell technologies to generate limitless supplies of replacement islets in the laboratory.
Vertex is furthest along. As reported in June, the company transplanted embryonic stem-cell-derived islets into 12 people with type 1 diabetes. After one year, ten participants no longer required insulin injections2. The company plans to seek regulatory approval for this cell therapy next year.
In a similar vein, scientists at regenerative-medicine company Reprogenix Bioscience in Hangzhou, China, are creating islets from reprogrammed stem cells derived from a recipient’s own fat tissue, with early reports of success3. Both approaches, however, still require recipients to take anti-rejection drugs, either to fend off immune attacks on donor cells or to counter the autoimmune assault that persists even against a person's own cells.
Stealth mode
Sana’s strategy aims to bypass the need for those drugs entirely. Company scientists began with islets from a deceased donor who did not have diabetes. Using CRISPR gene editing system, the researchers disabled two genes that normally help to flag foreign invaders to T cells, the immune system’s front-line defender. They then used a virus to shuttle genetic instructions for a protein called CD47 into the cells. This protein serves as a protective ‘do not eat me’ signal that prevents immune watchdogs, known as natural killer cells, from attacking the edited cells.
Enjoying our latest content?
Login or create an account to continue
- Access the most recent journalism from Nature's award-winning team
- Explore the latest features & opinion covering groundbreaking research
or
Sign in or create an accountdoi: https://doi.org/10.1038/d41586-025-02802-5
This story originally appeared on: Nature - Author:Elie Dolgin

















