If bird flu sparks a human pandemic, your past immunity could help

Older populations might be more protected than younger ones because of exposure to ‘matched’ strains during childhood, but an H5N1 pandemic is likely to take a major toll all the same
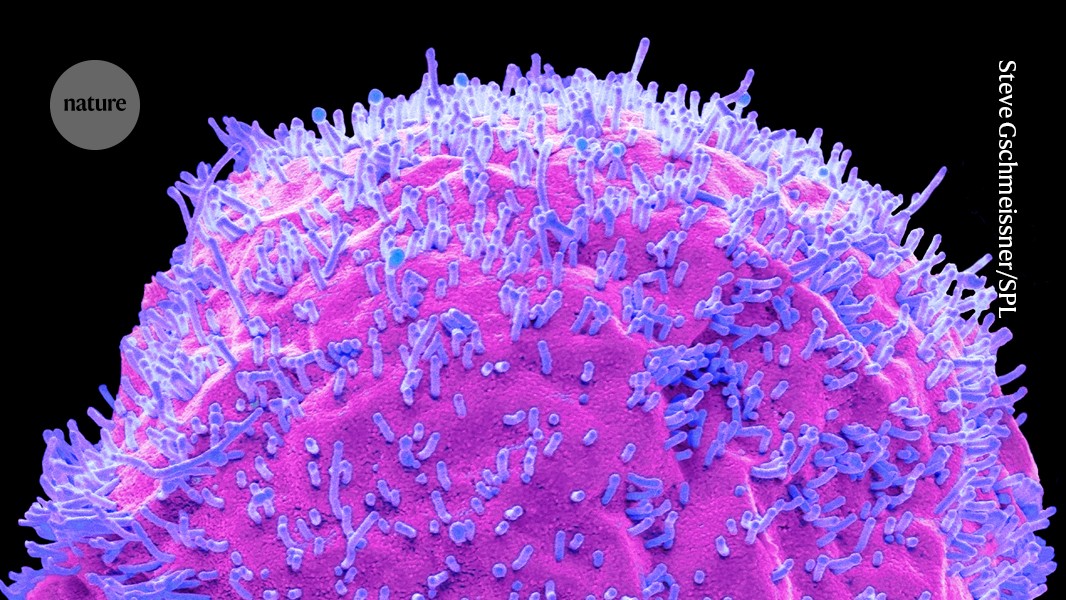
The bird-flu virus H5N1 (purple; artificially coloured) infects a human cell.Credit: Steve Gschmeissner/Science Photo Library
As the H5N1 bird-flu virus spreads relentlessly in animals around the world, researchers seeking to understand how a human H5N1 pandemic might unfold have turned to a rich source of clues: data on the immune system’s response to influenza.
Such information provides hints about who could be most vulnerable in an H5N1 pandemic. Previous research also suggests that, in a confrontation with the virus, our immune systems would not be starting from scratch — thanks to previous infections with, and vaccinations against, other forms of flu. But this immunity is unlikely to prevent H5N1 from inflicting serious damage to global health, if a pandemic were to begin.
From feathers to fur
The H5N1 strain now running rampant began as a bird pathogen before branching out to mammals. Classified as a ‘highly pathogenic’ virus for its lethality in birds, it has killed millions of domestic and wild birds around the world since it first emerged in 1996.1 It has also spread to a growing list of mammal species, including seals and foxes, and has caused more than 460 human deaths since 2003.
So far, the virus has not gained the ability to spread effectively between people, which has kept the potential for a pandemic at bay. But its repeated jumps from birds to mammals and evidence of transmission among mammals, such as elephant seals (Mirounga leonina)2, have alarmed researchers, who warn that the virus is gaining opportunities to become adept at spreading easily between people.
These worries were magnified when H5N1 was detected in March for the first time in US cattle — animals that interact frequently with humans. As of 8 July, US health officials have confirmed bird-flu infections in nearly 140 dairy herds in 12 states and in 4 dairy farm workers.
All of the workers had mild symptoms, but scientists caution that the virus is still a threat. It’s possible that the workers escaped severe illness because they might have caught H5N1 through exposure to milk from infected cows rather than the usual airborne particles, says Seema Lakdawala, an influenza virologist at Emory University School of Medicine in Atlanta, Georgia. Or perhaps it’s because the workers might have been infected through the eye rather than the typical route of the mouth or nose.
Malik Peiris, a virologist at the University of Hong Kong, says he is not surprised by these infections, “nor reassured that mildness of these cases means that this virus is inherently mild”.
Immune preparedness
The virus’s inherent virulence isn’t the only factor that would shape a pandemic, Peiris says. Another is the immune system’s state of readiness.
Through a combination of past infection and immunization, by the time people reach adulthood, they have generally had considerable exposure to flu. Some estimates3 suggest that up to half of younger populations are infected annually with ‘seasonal’ flu viruses, which cause regular waves of infections.
But exposure to seasonal flu offers limited protection against the new flu strains that could cause pandemics. These strains are genetically distinct from circulating seasonal strains, meaning that they face less built-up immunity in humans and can thus be more dangerous.
For now, H5N1 does not spread easily between people. But scientists worry that if it gains that ability, it could spark a pandemic, given that it is genetically different from seasonal flu viruses now in circulation. Tests of people across the United States found that few have antibodies against today’s strain of H5N1. This implies that “most of the population would be susceptible to infection from this virus if it were to start infecting people easily”, according to the US Centers for Disease Control and Prevention, which ran the tests.
Good news, bad news
That doesn’t leave people completely unprotected, because exposure to an older pandemic flu strain can defend against a newer one, says Michael Worobey, an evolutionary biologist at the University of Arizona in Tucson. For example, in a 2009 pandemic caused by the swine-flu virus H1N1, 80% of deaths were in people younger than 654. Older generations were spared owing to immunity stemming from exposure to different H1N1 strains when they were younger.
Exposure to H1N1 during the 2009 pandemic and at other times might, in turn, provide some protection against the H5N1 strain on the rise today. Both the H5N1 and H1N1 viruses have a surface protein designated N1, and an immune system that responds to H1N1 might also respond to H5N1. Peiris and his colleagues found that the near-universal exposure to H1N1 in 2009 and subsequent years produces antibodies that respond to H5N1 in nearly 97% of the samples they collected5. He is now running animal experiments to determine whether this antibody response confers protection against infection and serious illness.
All-important first flu case
There’s yet another complicating factor to the immune response to H5N1: a person’s first bout of flu might have an outsized effect on their future immunity. In a 2016 paper6, Worobey and his colleagues analysed almost two decades’ worth of severe infections caused by two subtypes of bird flu, H5N1 and H7N9. They found that people are generally unscathed by the flu strain that best ‘matches’ the one that had caused their first childhood flu infection — whereas they are more vulnerable to mismatched strains.
Thus, people born before 1968 have tended to escape H5N1’s ravages, because they probably had their first flu infection at a time when the dominant flu virus in circulation matched H5N1. But people born after 1968 eluded the worst of H7N9, because their first encounter with flu was probably with a virus that matched it rather than H5N1. Immunity from a first infection provided 75% protection against severe disease and 80% protection against death with a matching bird-flu virus, the authors found.
If an H5N1 outbreak were to occur, this first-bout effect predicts that older people could once again be largely spared and younger people could be more vulnerable, Worobey says. “We should have that somewhere between the back and front of our minds,” he says.
doi: https://doi.org/10.1038/d41586-024-02170-6
This story originally appeared on: Nature - Author:Max Kozlov

















