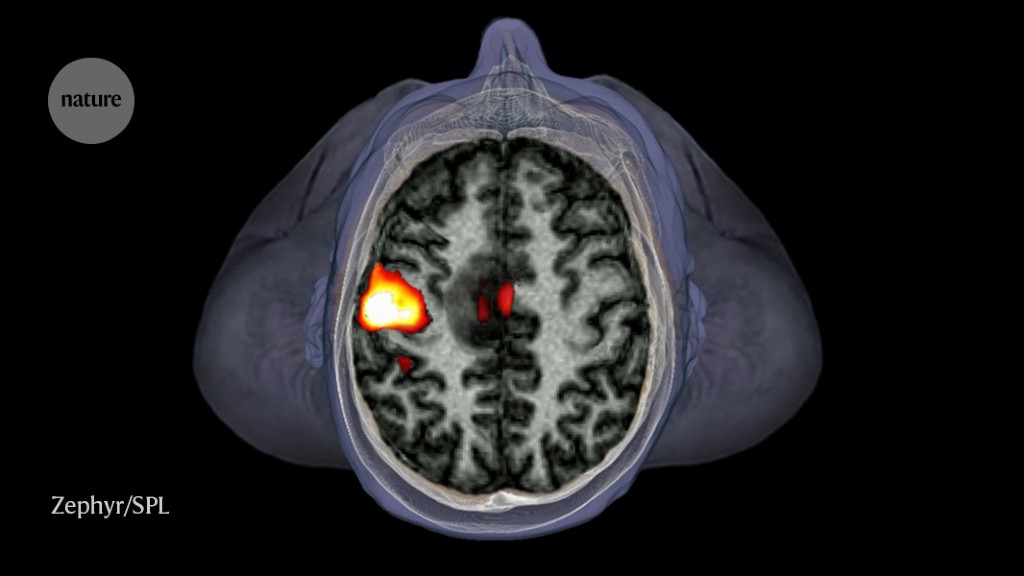
Brain imaging: fMRI advances make scans sharper and faster

Researchers are finding ways to improve one of neuroscientists’ favourite tools: functional magnetic resonance imaging
Last October, the neuroimaging community was abuzz with excitement. Researchers in South Korea seemed to have overcome one of the biggest limitations of functional magnetic resonance imaging (fMRI), a popular method for studying the human brain1.
Jang-Yeon Park, an author of the study, had been pondering the limitations of fMRI since his graduate student days at the University of Minnesota in Minneapolis. While conducting his PhD in medical physics, Park had developed a fascination for neuroscience. He found himself in seminars where researchers described studies of the human brain they had conducted with fMRI.
The technique works by picking up on changes in blood oxygen levels, which fluctuate with neuronal activity. But these blood-flow-related — or haemodynamic — changes are relatively slow compared with the neurons that they represent. To Park, this was a clear limitation. To reveal how the brain works, he thought, fMRI had to become much faster.
Typically, fMRI acquires brain slices as complete images — a process that limits how quickly the method can gather data. Instead, Park and his team at Sungkyunkwan University in Seoul tweaked the software to capture brain image data in segments, then used a computer algorithm to reconstruct the image. Using this modification — and a powerful MRI scanner — the researchers could track brain activity on the millisecond timescale, a temporal precision much greater that of conventional fMRI. This enabled them to detect the activity of mouse neurons from repeated stimulation of their whisker pads. The researchers published their technique1, which they dubbed direct imaging of neuronal activity (DIANA), in October 2022.
The rise of fMRI
DIANA is just one approach researchers have developed to improve fMRI. Some, such as Park, are devising ways to get closer to the neurons they wish to measure, rather than relying on the proxy measure of blood flow through the brain. Others have found improvements to fMRI’s spatial and temporal resolution — still relying on the blood-based signal — to capture more accurate snapshots of the brain in action.
“There are many promising avenues” that researchers have been exploring, says Noam Shemesh, an interdisciplinary MRI scientist at the Champalimaud Centre for the Unknown in Lisbon. “It’s all very exciting.”
The foundational principle of fMRI is neurovascular coupling — the idea that brain activity and blood flow are linked2. In 1880, the Italian physiologist Angelo Mosso, studying blood-flow variations in people with skull defects, observed that cognitive tasks could induce changes in blood flow3. Ten years later, British scientists Charles Roy and Charles Sherrington observed the effects of injecting brain extracts into the bloodstreams of animals. They hypothesized that metabolites produced by neuronal activity could increase blood flow to the brain4.
In 1990, Seiji Ogawa, then an investigator at AT&T Bell Laboratories in Murray Hill, New Jersey, and his colleagues noticed dark lines in the images of brains of rats and mice they had taken using MRI. These lines, they discovered, were blood vessels — the shadowy contours had formed because of deoxygenated haemoglobin (a protein that, when oxygenated, transports oxygen to cells throughout the body)5. Oxygenated and deoxygenated haemoglobin have different magnetic properties, and the drop in oxygenated blood led to an accompanying decrease in the MRI signal where the vessels were found. The researchers proposed that this blood-oxygen-level dependent (BOLD) signal could be exploited to measure brain activity5.
A few years later, three groups — including Ogawa and his colleagues — independently demonstrated that BOLD could detect brain activation in humans in MRI scanners6–8, yielding the method researchers now call fMRI.
It provided a clear advantage over other neuroimaging techniques. Although electroencephalography (EEG), which measures brain electrical activity, and magnetoencephalography (MEG), which records magnetic fields produced by neuronal activity, collect data much more rapidly than fMRI does — picking up signals on a millisecond, rather than second, timescale — fMRI is better at pinpointing where in the brain the activity occurred. And unlike with positron emission tomography, there is no need to inject radioactive substances into the bloodstream.
MRI was already a popular tool for creating detailed anatomical images in medicine, and MRI scanners were available in hospitals around the world. fMRI could be conducted simply by applying new software to these existing machines. “We could just ride on the back of the success that MRI was already experiencing,” says Peter Bandettini, a physicist and neuroscientist at the National Institute of Mental Health in Bethesda, Maryland. “The field propagated so quickly and easily because of that.” Now, researchers publish more than 10,000 academic articles mentioning fMRI annually.
Still, the technique has limitations. One is that it does not directly measure brain activity. It can take seconds for blood oxygenation changes to occur, whereas neurons fire on millisecond timescales. This raises the question of how exactly neural activity leads to changes in blood oxygen levels — and whether the relationship between neuronal activity and blood oxygenation is the same throughout the brain.
fMRI also struggles to image diseases in which blood flow is affected, such as cardiovascular disease or Alzheimer’s disease. Because BOLD-based fMRI measures changes in blood flow, it cannot distinguish a vascular abnormality from a neuronal one. This poses a problem for both understanding and treating disease, says Shella Keilholz, an MRI physicist and neuroscientist at Emory University and the Georgia Institute of Technology, both in Atlanta.
Imaging at the neuronal level
Some researchers are searching for alternative ways to measure brain function — and especially, to detect neuronal activity directly.
One method, neural current imaging, measures the electromagnetic fields generated by neuronal electrical activity, similar to what EEG or MEG can do. The fields produced are much smaller than that created by the BOLD effect, says Bruce Rosen, a physicist and radiologist at Harvard Medical School in Boston, Massachusetts, making them hard to spot using MRI. Researchers have demonstrated that the approach is theoretically possible — showing, for example, that electromagnetic signals can be detected using MRI in post-mortem turtle brains9–10. In human brains, however, scientists have had little success.
Researchers have also tried to detect neuronal function by tracking physiological changes. When neurons receive input from other activated neurons, they swell temporarily. This can be detected using diffusion MRI, a technique that measures the movement of water molecules. Denis Le Bihan, a neuroscientist and physicist at NeuroSpin, a research institute in Paris aimed at advancing MRI, says that although the exact mechanism through which diffusion MRI detects changes in neuronal swelling remains an open question, one potential explanation is that cell swelling alters how water molecules organize around neuronal membranes.
Increasingly powerful scanners for magnetic resonance imaging are becoming available, enabling improved resolution in brain scans.Credit: Jens Schlueter/DDP/AFP via Getty
Diffusion MRI, which Le Bihan developed in the 1980s11, is used in the clinic to detect strokes and other brain diseases. It is also the basis for diffusion tensor imaging, which researchers use to map the organization of white matter in the brain. But the ability to detect neuronal function with this method, dubbed diffusion fMRI — which Le Bihan and his colleagues first reported in the 2000s12,13 — has faced scepticism. Researchers have questioned whether diffusion fMRI is identifying the morphological changes that occur with neuronal firing, or if it is simply picking up on changes in blood flow.
Le Bihan and others have worked to convince the neuroimaging community that diffusion fMRI can indeed pick up on cell swelling that is linked to neuronal activity. Shemesh, for instance, says that work from his group in the past few years5 provides clear evidence of this. “We saw signals that are just too fast to be related to blood flow — and they coincide with measurements of morphological changes of activity,” he explains.
Still, the technique has yet to be adopted widely. For one thing, diffusion fMRI produces a weaker signal than BOLD-based imaging does. It also requires scientists to learn how to use new software. More to the point, researchers have yet to be convinced of the utility of diffusion fMRI, says Keilholz. Demonstrating that this technique produces different results to BOLD in patients with diseases such as Alzheimer’s could drive adoption, she says.
A new view of the brain
For her part, Keilholz is convinced of diffusion fMRI’s potential. She says she regarded the method as the most promising for directly detecting neuronal activity — until Park’s method from South Korea came along, that is.
As Park explains, the technical background for his approach dates back to 2014. Soon after he joined the faculty at Sungkyunkwan University in Seoul, he came across a paper by researchers at the National Institute of Neurological Disorders and Stroke in Bethesda that reported a unique way of acquiring fMRI data14. It enabled the researchers to gather data with 40- to 50-millisecond resolution — much faster than conventional fMRI — and they used it to study neuronal activity in specific cortical layers of the rat brain. Park thought he might be able to apply the method to push the temporal resolution further, up to the speed at which neuronal firing occurs.
His modifications to the imaging software led to an increase in temporal resolution to 5 milliseconds. This enabled the team to detect neuronal activity generated by repeatedly stimulating the animal’s whisker pads in two regions — the somatosensory cortex, which processes sensory inputs, and the thalamus, a relay station for sensory and motor inputs1.
According to Yen-Yu Shih, a neuroimaging scientist at the University of North Carolina School of Medicine in Chapel Hill, DIANA could represent a breakthrough in temporal resolution in fMRI. Although more work needs to be done before the method can be widely adopted, Shih says, “even showing that there’s a possibility is already a tremendous contribution to the field”.
Still, experts caution that it is still too early to determine how useful the technique will be.
First, there are its limitations, Bandettini says. The signal that DIANA produces is small relative to BOLD-based fMRI, meaning it can be difficult to detect. The technique is also highly sensitive to motion — the animals in Park’s study were anaesthetized — and requires the stimulus (in this case, the electrical stimulation of whisker pads) to be precisely synchronized with data acquisition. That could limit the method’s applications to processes such as vision, hearing or touch, in which it is possible to provide stimuli at regular intervals. Higher-level cognitive functions, such as memory, might be more difficult to capture in this manner.
There is also the question of what the researchers are detecting with DIANA. Park and his colleagues suggest that they are picking up on changes to the water molecules on the surface of neurons. Park says that changes in the membrane ‘potential’ — the concentration of charged ions on either side of the cellular membrane — alter the hydration on the cell surface. An MRI scanner, which senses changes in water molecules, might be able to detect that difference. Another possibility, he says, is cell swelling, which diffusion MRI can also detect. Le Bihan notes that both effects could be happening, because cell swelling might be related to the water layer around the cell membrane. However, he and other specialists say that the jury is still out on which, if either, of these factors underlies the effects that Park and his team observed.
Technical improvements could theoretically resolve these issues, Bandettini says, but the biggest question right now is whether other groups are able to replicate Park’s results independently. “I think the enthusiasm about this should be tempered until we know more about the nature of the signal we’re looking at and we can get some reproducing results,” Bandettini says. However, he adds, “if we figure out a way to make DIANA work well, it would be huge”.
Park says he and his team are now working to optimize data acquisition and analysis — and to implement DIANA fMRI in humans. “That’s the highest priority,” he says.
Building better BOLD
In the meantime, researchers have also devised ways to improve fMRI without abandoning neurovascular coupling.
One key advance comes down to the hardware. More powerful magnets mean researchers can collect better data, because they reduce the signal-to-noise ratio and enable images to be obtained at higher spatial and temporal resolutions. Some of the first human fMRI studies were done using magnets with field strengths of 1.5 tesla, about 30,000 times stronger than Earth’s magnetic field. Scientists have now used magnets of up to 10.5 tesla in human neuroimaging studies, and ever more powerful ones are being built. In February, a consortium of research institutions in the Netherlands announced that it would construct the world’s strongest human MRI scanner so far, a machine with a magnetic field strength of 14 tesla.
Researchers have also varied the ways in which they observe blood flow through the brain. Because BOLD depends on changes in blood oxygen levels, it’s more sensitive to blood flow through large veins, which drain deoxygenated blood away from the sites where brain activity occurred, than through regions with smaller vessels, such as capillaries. This becomes an issue when researchers want to look at the brain in finer detail. To get around this problem, researchers developed techniques such as vascular space occupancy15, which measure changes in blood volume rather than blood oxygenation. Such tools have enabled neuroscientists to obtain better spatial resolution than with standard BOLD fMRI, making it possible to look at differences in neuronal activity across various layers of the brain’s cortex16.
Other improvements include updating data-collection techniques and using machine learning to improve image reconstruction. Some scientists are working on improving their understanding of the BOLD signal itself. Even after 30 years, many questions about BOLD-based imaging remain, Shih says, such as whether neurovascular coupling occurs in the same way across brain regions, and how the haemodynamic signal is influenced by the activity of different cell types or molecules such as neurotransmitters.
Anna Devor, a biomedical engineer at Boston University in Massachusetts, and her colleagues are looking at how changes in blood flow are linked to fluctuations in neurotransmitters. “Today, if you look at the functional MRI maps, you’ll see where the activity is happening, but you don’t know what the activity is,” Devor says. “We’re trying to figure out how these patterns of haemodynamics are related to specific neuronal circuits.”
The reality is that, although techniques such as DIANA stir up excitement in the neuroimaging field, BOLD is here to stay, at least for the foreseeable future. “We’re always looking for something that works better than BOLD,” Bandettini says. But BOLD has been “amazingly robust” for so many neuroscience questions. “I think that there will still be more surprises and insights to be gained,” he says.
Nature 617, 640-642 (2023)
doi: https://doi.org/10.1038/d41586-023-01616-7
This story originally appeared on: Nature - Author:Diana Kwon


















