Hope, despair and CRISPR — the race to save one woman’s life The efforts hold lessons for the messy state of modern drug development

Researchers in India fought to develop what could have been the first therapy to use gene-editing to halt a rare neurodegenerative disease
When researcher Arkasubhra Ghosh finally met Uditi Saraf, he hoped that there was still a chance to save her.
Ghosh and his collaborators were racing to design a one-off treatment that would edit the DNA in the 20-year-old woman’s brain cells and get them to stop producing toxic proteins. It was an approach that had never been tried before, with a long list of reasons for why it might not work.
But the team was making swift progress. The researchers were maybe six months away from being ready to give Uditi the therapy, Ghosh told her parents over breakfast at their home outside New Delhi last June. Even so, Uditi’s mother was not satisfied. Work faster, she urged him.
Then, Uditi was carried to the breakfast table, and Ghosh understood her urgency. Once a gregarious and energetic child and teenager, with a quick laugh and a mischievous streak, Uditi was now unable to walk or feed herself. She had become nearly blind and deaf. Her family tried to talk to her: “These are the people who are making a therapy for you,” they said loudly.
Shaken, Ghosh returned to his gene-therapy laboratory at Narayana Nethralaya Eye Hospital in Bengaluru, India, and got to work. “If you need to put up tents in the lab, then we can do so,” he told his students. “I’m not going to sleep.”
Four months later, Uditi was gone.
The first therapy using CRISPR genome editing was approved in late 2023 to treat blood disorders that affect thousands of people worldwide. But the approach is also a source of hope to many people who have extremely rare genetic conditions, like the one Uditi had. Genome editing could one day become a radical way to address the diseases that are overlooked by pharmaceutical companies. “Patients are waiting, families are waiting,” says Jennifer Doudna, a molecular biologist at the University of California, Berkeley. “So we need to get on with it.”
Researchers are still laying the groundwork for this future. They are working out how best to design and manufacture the treatments, and how to deliver them to precise locations in the body. The cost is also a problem: the price of genome-editing therapy threatens to put it out of reach for many. Ghosh wants to bring those barriers down, and he’s convinced that India will eventually be the country to do it.
But Uditi’s family could not wait — the pace of scientific research was too slow. They needed a sprint, and a team of researchers willing to take on not only the scientific challenge, but also the emotional heft and high risk of failure involved in attempting something that had never been done. “What we were trying to do was really almost in the realms of science fiction,” Ghosh says.
And he remains convinced that, despite Uditi’s tragic death, the lessons learnt will help others on a similar path. “It truly is a story of hope.”
A crushing diagnosis
As a young girl, Uditi was always in a hurry. Seizing any excuse to celebrate — whether it was a birthday or a festival — she would buzz around the house getting ready hours ahead of everyone else, peppering her mother with urgent requests. She greeted family and friends with cuddles and kisses and brightened parties with her laughter and dancing.
For the first nine years, there was no hint of trouble. And when it began, it was just a flicker — a few seconds here and there, when Uditi would zone out.
She’d switch back on again as if nothing had happened, and her mother, Sonam, wasn’t sure if she should worry. But then Sonam saw nine-year-old Uditi drop a camera on the floor and become confused as to why it was no longer in her hand. A mother’s hunch hardened: something was wrong.
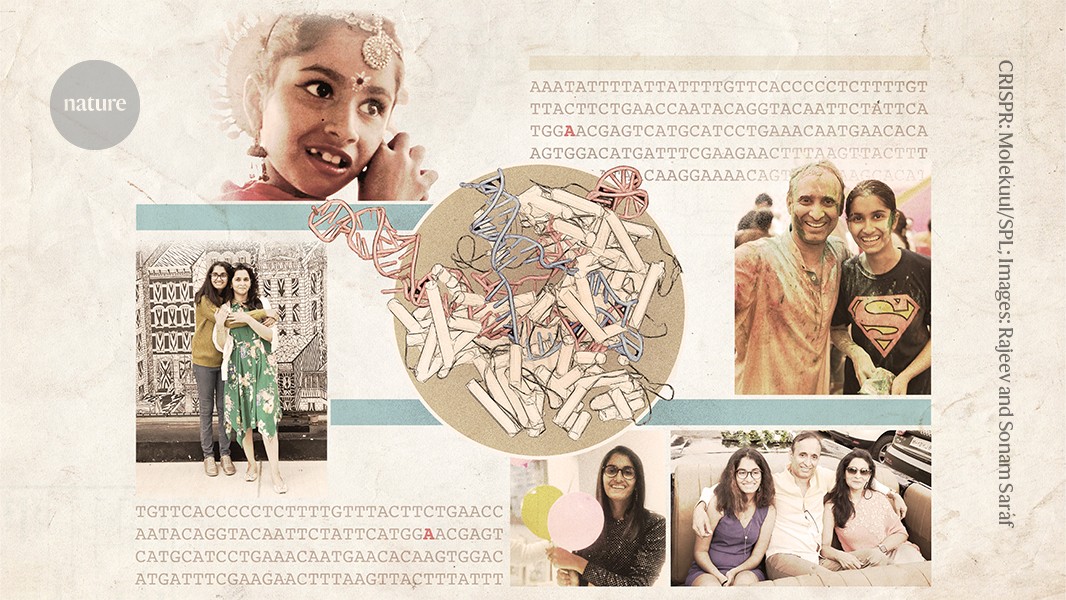
Uditi Saraf with her mother, Sonam Saraf.Credit: Rajeev and Sonam Saraf
The physicians diagnosed her with epilepsy. When Uditi’s seizures became more pronounced and she began to struggle at school, Sonam and Rajeev, Uditi’s father, decided it must be something more. In 2017, they had part of Uditi’s genome sequenced.
It was a deviation from the standard treatment path, but the Sarafs were technologically savvy and financially well off. In India, as in many places in the world, genome sequencing was still uncommon, its roll-out slowed both by the costs and by the dearth of genetic information from people of Indian descent in genetic databases. Without such data, it can be difficult to interpret sequencing results.
Uditi’s results, however, were unambiguous: a single-base change in the gene that codes for a protein called neuroserpin caused tangled polymers to form in her brain cells, interfering with their function. Uditi’s neurons were dying.
This condition is called FENIB (familial encephalopathy with neuroserpin inclusion bodies), and the symptoms — which can be similar to dementia — usually manifest late in life. Elena Miranda, a cell biologist at the Sapienza University of Rome, runs the world’s only lab that focuses on the disease. She says that it’s possible that many cases of FENIB go unreported because physicians do not often sequence the genomes of older adults with dementia.
But the most severe forms of FENIB strike early and are exceedingly rare. Miranda has known of only three other people with the same mutation that Uditi had. “This form of the disease is very aggressive,” she says.
Uditi and her parents embarked on a lonely journey familiar to many people with rare diseases. They had never heard of FENIB, and neither had Uditi’s physicians. Sonam did some research but couldn’t bring herself to fully absorb what she found. “We thought it’s not possible,” she says. “It cannot happen with our daughter.”
The Sarafs studied what they could find online and tried the interventions available to them: Indian ayurvedic treatments, a ketogenic diet, special schools, seeing a slew of physicians and trying out various medicines. “We shopped for doctors. We shopped for gods,” says Sonam, but Uditi’s condition slowly worsened.
The three moved to upstate New York in 2018 to send Uditi to a school for people with disabilities. Her seizures intensified, and frequent muscle spasms made it hard for her to walk or drink from a glass. Her bright personality was dimming. The Sarafs discussed experimental treatments with Uditi’s new physician, epilepsy specialist Orrin Devinsky at NYU Langone Health in New York City. Devinsky mentioned a couple of options, one of which was CRISPR genome editing. Rajeev seized on the idea.
Uditi’s disease was caused by a mutation that converts a single DNA base from a ‘G’ to an ‘A’. A variation on CRISPR genome editing, called base editing, could theoretically correct exactly this kind of mutation (see ‘Precision gene repair’).

Devinsky also emphasized the difficulties. At that time, base editing — which was first reported in 2016 — had never been tested in a clinical trial. The technique requires shuttling a relatively large protein and a snippet of RNA into affected cells. Researchers were struggling with how to perfect this delivery for many organs — the brain being one of the most daunting.
Even if each of these hurdles were surmounted, at best, base editing might stop the production of neuroserpin clumps in some of Uditi’s neurons. The treatment was unlikely to reach all affected cells, and it was unlikely to clear the clumps that were already present or to regenerate neurons that had been lost.
But Rajeev and Sonam saw an opportunity for hope: perhaps such a therapy could slow down the progression of Uditi’s disease, buying time for scientists to develop another treatment that could repair the damage that had been done. The Sarafs were on board.
New York to New Delhi
Devinsky assembled a team at NYU Langone Health with expertise in genome editing and neuroscience to conduct preliminary studies of the approach. The researchers pulled together what funding they could from other grants, and the Sarafs funded the rest. “We will sell our house if we have to,” Sonam said.
The pressure in the lab was intense, says team member Jayeeta Basu, a neuroscientist at NYU Langone Health. The team genetically engineered Uditi’s FENIB mutation into cells grown in the lab. When the cells initially didn’t seem to behave as expected, Basu asked her graduate student to repeat the experiment five times. “I was always pushing,” she says. “We had to be fast, but we also had to be diligent. There was no short cut.”

Rajeev Saraf with his daughter Uditi.Credit: Rajeev and Sonam Saraf
In December 2019, the Sarafs moved back to India. Maintaining a home in the United States was expensive, and Uditi missed her extended family. Then the COVID-19 pandemic struck, and in January 2021, Uditi was hospitalized with severe COVID-19. She spent 20 days in the hospital and her health was never the same, says Sonam. Communication became increasingly difficult for Uditi and she began to pace the house incessantly, rarely even going to sleep.
The Sarafs decided to speed up the base-editing project by funding a second team in India.
Meanwhile, Devinsky had petitioned a US foundation to devise a different experimental treatment called antisense therapy for Uditi. The family flew from India to the United States twice for injections into her spine. The trips became traumatic as her ability to understand the world around her declined.
The treatments didn’t work. And the experience taught Rajeev and Sonam how long it could take to get approval to try an experimental therapy in the United States. They decided Uditi’s base-editing therapy should also be manufactured and administered in India.
About an hour and a half away from their home, Debojyoti Chakraborty, a geneticist at the Council of Scientific and Industrial Research’s Institute of Genomics and Integrative Biology in New Delhi, had been making headlines for his efforts to devise a CRISPR-based treatment for a genetic blood disorder called sickle-cell disease.
Researchers in the United States were also developing genome-editing therapies for sickle-cell disease, but those therapies were expected to be expensive and potentially out of reach for much of the world. (The UK Medicines and Healthcare Products Regulatory Agency approved the first one, Casgevy, made by Vertex Pharmaceuticals in Boston, Massachusetts, and CRISPR Therapeutics in Zug, Switzerland, which costs US$2.2 million per patient.)
Most of the people with sickle-cell disease in India — a country with one of the highest rates of the condition — live in impoverished communities. Chakraborty and his colleagues hoped to develop a therapy that could be produced and administered at a fraction of the price that is charged in the United States, if not less.

Debojyoti Chakraborty is trying to develop affordable CRISPR-based treatments in India.Credit: RNA Biology Lab
Rajeev and Sonam went to the institute to talk to Chakraborty and the institute’s director, chemist Souvik Maiti, who had been collaborating with Chakraborty on the CRISPR technology behind the sickle-cell project.
Although the institute gets many requests for help from people with rare diseases and their caregivers, the Sarafs were unusual in that they would be able to help fund the work, says Maiti. Uditi was the only person in India known to have her neuroserpin mutation, and no government agency, company or philanthropy was likely to pay for the development of a treatment. “It’s very difficult,” Maiti says. “Even if our heart is telling us we should work on it, until there is funding, we cannot do it.”
Even with funding, Maiti and Chakraborty took some time to discuss the project with Ghosh, who was building a facility in Bengaluru to produce viruses called adeno-associated viruses (AAVs), which are often used in gene therapies. Ghosh aimed for his facility to be one of the first in India to produce AAVs to the standards required for use in people.
There were a lot of unknowns in the base-editing project. And in addition to the work on stem cells in the lab, the team would need to do further experiments to determine which base-editing systems would work best, where and how to deliver its components into the body, and whether the process generated any unwanted changes to the DNA sequence. They would need to do experiments in mice to test the safety and efficacy of the treatment. They also needed to get Ghosh’s facility approved by India’s regulators for producing the base-editing components.
A race to reduce costs
Uditi’s illness had probably already progressed beyond the point at which the therapy could offer a notable benefit, but the family wanted them to try, reasoning that the work that they did on this project could help future endeavours to develop genome-editing therapies for genetic conditions.
It was not the first time Ghosh was swayed by a personal appeal: a few years before he met Uditi, Ghosh came to work and found two women waiting outside of his office. They would not leave, the women said, until he committed to finding a treatment for their young sons’ illness, a genetic condition called Duchenne muscular dystrophy, which can be fatal. The women pledged to help raise funds, and Ghosh found himself unable to say no. He has worked on the project and grown close to the families since then.
Lab protocols for making medicines are notoriously strict, with each step carefully controlled to minimize the chance of contamination. When setting up his facility for manufacturing gene therapies, Ghosh scrutinized each step, looking for ways to cut costs without sacrificing safety, arguing his case to India’s regulators. He estimates that gene therapies for eye diseases that are developed in his lab will one day be available for one-hundredth of what they cost in the United States. “We will certainly short circuit this entire field,” Ghosh says.
India has earned a reputation for making complex drugs on a budget. During the COVID-19 pandemic, Indian manufacturers cranked out millions of doses of vaccines. Now, the country is manufacturing a malaria vaccine at a fraction of the cost of that in Europe, and it is developing sophisticated cell and gene therapies used in cancer treatments for much less than the price of those in the United States.
Chakraborty took the lead on Uditi’s project. “He is a go-getter kind of person,” says Riya Rauthan, who was then a PhD student in Chakraborty’s lab. “He is not bothered by who he needs to ask to get something done, he just does it.”
To minimize interruptions, the team mapped out all of the experiments and the components they would need from start to finish. In India, many lab reagents have to be imported, and supply interruptions can delay projects by weeks or months. Everything had to be planned and ordered ahead of time, and Maiti worked to keep the supplies coming, seeking out vendors and negotiating prices. “Time was more valuable than anything else,” he says.
One of the most important reagents had to come from abroad: antibodies that could recognize the neuroserpin protein and its tangles. Few researchers use such antibodies, and the supply was uncertain. The team decided that the quickest way to get reliable antibodies was to ask Miranda in Rome to share the ones she had developed. She gladly did. “This was a desperate approach,” she says. “But for me the priority was to try to help as much as I could.”
Rauthan generated stem cells from samples of Uditi’s blood. Then, she and her colleagues coaxed those cells to become neurons, and used base editing on them in the lab.

Arkasubhra Ghosh is building an Indian facility to make viral vectors for gene therapy.Credit: Arkasubhra Ghosh
Ghosh worked on preparing the AAV that would be used to transport the CRISPR components into Uditi’s neurons. The team needed to determine which strain of AAV would work best — some strains could trigger inflammation in the brain. Ghosh’s lab tested several types of AAV in mice, to find out which one caused the least amount of inflammation and how best to administer it. The team eventually settled on one type — called AAV9 — and determined that it should be injected directly into Uditi’s brain.
Still, that was not the end of their challenges. AAV genomes can carry only an extra 4,700 DNA bases, but the gene that codes for the enzyme needed in base editing is longer than that. Ghosh and his students worked to divide up their genomic cargo so that it could fit in two separate viruses, and added sequences that would allow the two pieces to be spliced together again when they are expressed inside a cell. The team would inject both viruses at the same time.
The approach has been shown to work in mice but had not yet been tested in humans (J. M. Levy et al. Nature Biomed. Eng. 4, 97–110; 2020).
By June 2023, the team seemed to be barrelling towards the finish line. Many of the researchers were working 10-to-12-hour days, and it was nearly time to test their therapy in mice. Ghosh was also scheduling a regulatory inspection to ensure that he would have the approvals he needed by the time the animal results were in. A surgeon had agreed to perform Uditi’s injection.
If all went well, they might be ready to treat Uditi in as little as six months, Chakraborty predicted.
Pushing past tragedy
In early October, a few months after Chakraborty and Ghosh had breakfast with Uditi and her parents, the team received a series of messages from Rajeev on their WhatsApp group. Uditi had become ill with pneumonia and had been taken to the hospital. Then she was in a coma and had been sent home — there was nothing else the physicians could do for her.
Soon afterwards came the message they had all feared: Uditi was gone.
Ghosh thought immediately of the two little boys with Duchenne muscular dystrophy: “What if I’m too late for them, too?”
Others in the lab also took the news hard. “For clinicians, perhaps they become hardened,” says Chakraborty. “We don’t have that experience. We were feeling agony.”
Ten days after learning that Uditi died, Chakraborty presented the lab’s efforts at a local conference and finished his talk with a picture of Uditi, smiling. In the audience, Riya Patra, a graduate student in Ghosh’s lab, began to cry. It was the first time she’d let herself see a picture of the young woman she’d tried so hard to save. “Before, I had thought that if I saw her, maybe I would cry,” she says. “And I wouldn’t be able to work anymore.”
An estimated 100 million people in India have a rare disease. For decades, people affected by such conditions have cycled through hope and disappointment as researchers have inched closer to developing therapies that can help them at a genetic level. After a series of sporadic starts and failures, gene therapy has finally begun to find its footing. This has set the stage for CRISPR-based genome editing to rocket to the clinic.
When nine-year-old Uditi first dropped her camera, CRISPR was just an oddity — a strange assembly of sequences found in microbial genomes, only studied by a few die-hard microbiologists. Four years before she was diagnosed with FENIB, researchers showed for the first time that a CRISPR-based system could cut DNA in human cells grown in the lab. And the first CRISPR-based genome-editing therapy was approved in the United Kingdom to treat sickle-cell disease the month after Uditi died.
In theory, many people with a genetic condition, no matter how rare, could benefit from these technologies. But the reality is harsher. It will take years to establish the techniques needed to create rapid, on-demand, bespoke CRISPR therapies. Most people with these conditions don’t have that kind of time.
But researchers are working to streamline the process. Doudna’s institute, for example, is working to standardize some aspects of genome-editing therapies, in part to make it cheaper and easier to develop such treatments for people with rare conditions. And the US National Institutes of Health has been trying to develop similar pipelines for gene therapies — an effort that could help to inform genome-editing efforts. “It’s been really hard,” says Doudna. “But what we’re doing is going to have long-term impact.”
In India, the work has continued. Rajeev has urged Chakraborty to finish the team’s studies in mice, so that the next person with FENIB will not have to wait as long for a potential treatment. Some of the work will be completed, and the effort could benefit others with genetic conditions that affect the brain — particularly in India. “We are not really trying as aggressively as we did earlier,” he says. “But that technology has a lot of potential.”
At Uditi’s memorial service, Rajeev tried to make sense of the timing. Uditi was always in a hurry, he told attendees. She always had to be first. She was only a few months away from receiving an experimental treatment, but she would not wait, not even for that. “She could not let science win,” he said. “She was always ahead.”
Nature 630, 284-288 (2024)
doi: https://doi.org/10.1038/d41586-024-01716-y
This story originally appeared on: Nature - Author:Heidi Ledford


















