What causes long COVID? Case builds for rogue antibodies

Study finds that antibodies from people with the debilitating condition trigger similar symptoms in mice
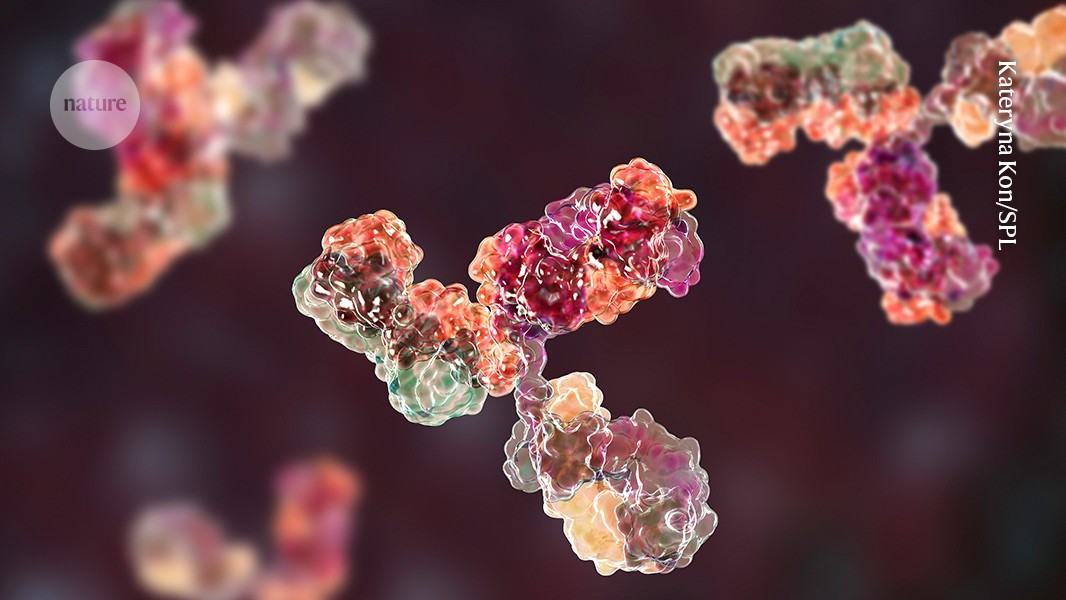
IgG antibodies (artist rendering shown here) taken from people with long COVID and injected into mice give the animals symptoms such as increased pain sensitivity and reduced motor function.Credit: Kateryna Kon/Science Photo Library
Antibodies isolated from people with long COVID increase pain sensitivity and reduce movement in mice when transferred to the animals, research shows1. The findings suggest that antibodies might drive some symptoms of long COVID — although how that process works is unclear, and the results will need to be replicated in larger studies.
“I think this will be a beacon of a paper that we can take forwards to further understand long COVID,” says Resia Pretorius, an immunologist at Stellenbosch University in South Africa.
Previous research has hinted that long COVID might be caused, at least in part, by autoantibodies — rogue antibodies that a person generates that attack their own immune system or tissues. But one big question remained: “Is it really causal?” says Jeroen den Dunnen, an infectious-disease researcher at the Amsterdam University Medical Center. In other words, do autoantibodies cause long COVID symptoms, or are they simply generated in response to a long COVID infection? Along with his colleagues, den Dunnen undertook the latest study to get an answer.
Complex picture
Scientists estimate that around 10–20% of people who are infected with the SARS-CoV-2 coronavirus will develop long COVID — a severe condition whose symptoms, including intense fatigue, debilitating brain fog and chronic pain, persist for at least three months after the initial infection. The condition affects at least 65 million people worldwide, but researchers still have little understanding of its causes, and there are no proven treatments.
Some studies suggest that long COVID might be caused by persistence of SARS-CoV-2 in the body2. Others indicate that it could arise from tiny blood clots that block blood vessels and limit oxygen exchange in a person’s body3. And then there is the autoantibody hypothesis.
To explore that mechanism, den Dunnen and his co-workers collected IgG antibodies — the most common type of antibody in human bodily fluids — from blood taken from 34 people. Participants were 43 years old, on average, and developed long COVID after having mild SARS-CoV-2 infections during the first two years of the pandemic. Most participants in the study, which was posted last month ahead of peer review to the preprint server bioRxiv1, experienced fatigue and chronic pain and had to take time off work owing to their condition.
The researchers assigned the participants to groups on the basis of the concentrations of various inflammatory proteins in their blood, and pooled antibodies from members of each group. They then injected each mouse with one of the pools.
The various antibody groups had distinct effects on pain perception and motor activity in the mice, says co-author Niels Eijkelkamp, an immunologist at the University Medical Center Utrecht in the Netherlands.
The researchers discovered that mice injected with antibodies from two groups of people with long COVID were more sensitive to being pricked on the paw than were mice injected with antibodies from people who had fully recovered from mild COVID-19. There were no changes in motor function between these two groups and the control group, however.
But when given antibodies from a third group of people with long COVID, mice walking for half an hour covered 40% less distance, on average, than did animals in the control group. And this group of animals had no change in pain sensitivity compared with control animals. This suggests that antibodies from people with long COVID can trigger a range of symptoms in mice, Eijkelkamp says. He and his colleagues think that the antibodies might cause such effects by attacking healthy tissue.
Beacon of hope
This study is really picking up “the mood music in long COVID research”, says Peter Openshaw, a physician and immunologist at Imperial College London, because it is adding to a growing body of evidence that autoimmunity factors into the disease. But it is based on “a relatively small number” of participants and therefore needs to be reproduced independently, he adds.
That seems to have already happened, at least on a small scale. In a webinar hosted last month by Solve M.E., a non-profit organization based in Glendale, California, that supports long COVID research, David Putrino, a physiotherapist at the Icahn School of Medicine at Mount Sinai in New York City, discussed the results of a similar study, in which researchers injected mice with IgG antibodies from people with long COVID. These mice had increased pain sensitivity compared with those injected with antibodies from healthy people. “It’s great to see that it’s reproducible,” den Dunnen says.
If the findings hold, clinicians might want to consider excluding individuals with long COVID from making blood donations, says Davide Robbiani, an immunologist at the Institute for Research in Biomedicine in Bellinzona, Switzerland.
But the results might also present a new animal model for studying long COVID, says Pretorius, who is now collaborating with den Dunnen and Eijkelkamp to investigate the role of microclots in the disease.
Danny Altmann, an immunologist at Imperial College London, is more sceptical. “Things like long COVID are really, really hard to reiterate in animal models,” he says, and it is unclear how well the symptoms observed in mice really reflect what’s going on in humans. “We’ve invested almost zero in building up those models,” he says, owing to a lack of government interest and “policymaker fatigue” in funding long COVID research. So even “if this study catalyses debate about the vacuum of small-animal models that are really holding back the field, I think it’s helpful”, he adds.
doi: https://doi.org/10.1038/d41586-024-02010-7
This story originally appeared on: Nature - Author:Carissa Wong


















