Debate rages over Alzheimer’s drug lecanemab as UK limits approval

The medicine is being assessed by agencies including the European Union regulator, but the community is divided on its efficacy and safety
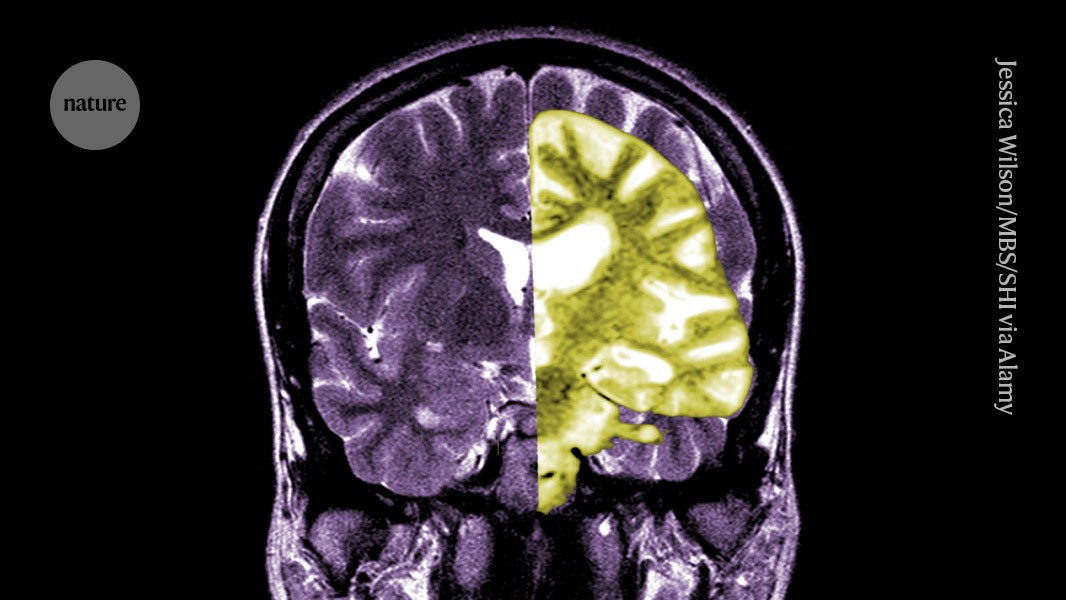
A composite MRI image showing a healthy brain (left) and one with advanced Alzheimer’s disease (right).Credit: Jessica Wilson/Medical Body Scans/Science History Images via Alamy
Debate over the Alzheimer’s disease drug lecanemab — one of the first to slow cognitive decline in people — is intensifying among researchers and clinicians over whether the potential benefits of treatment outweigh the risks of harm.
On 22 August, the UK Medicines and Healthcare products Regulatory Agency greenlit the drug. But at the same time, the UK healthcare regulator NICE, which determines whether drugs will be offered to patients on the government-funded UK National Health Service (NHS), said in draft guidance that lecanemab will not be made available on the NHS because the benefits are too small to justify the high cost.
“The unusually long time that they have spent considering the drug suggests that this has not been an easy or straightforward decision,” said psychiatrist Robert Howard at University College London in a statement to the UK Science Media Centre.
US regulators were the first to authorize the drug in 2023, and the European Medicines Agency (EMA) is now reassessing its decision following an appeal by the drugmaker.
Amyloid target
The EMA’s decision was also met with mixed responses from the Alzheimer’s community. “Emotions are really high here,” says Christian Haass, a biochemist at the Ludwig Maximilian University in Munich, Germany, who disagrees with the decision. “It’s the first disease-modifying drug we have in more than 30 years.” Denying patients the ability to access lecanemab means many will lose out on the opportunity to gain valuable time, he adds.
Lecanemab, or Leqembi, is a monoclonal antibody that works by clearing amyloid, a substance that builds up into toxic clumps in the brains of people with Alzheimer’s disease. The drug, which is made by Eisai in Tokyo and Biogen in Cambridge, Massachusetts, is also approved in China, Japan, South Korea and the United Arab Emirates.
Others applaud the EMA and say that while the drug did effectively lower amyloid levels in the brain, whether the reduction in cognitive decline it led to will result in clinically meaningful benefits for patients remains unclear. They say that the possibility of serious complications such as bleeding or swelling in the brain caused by a side effect known as amyloid-related imaging abnormalities (ARIA), although small, is a big concern. “Any reasonable assessment of the risks versus the benefit of this drug should lead people to be very sceptical of it,” says Matthew Schrag , a neurologist at Vanderbilt University in Nashville, Tennessee.
Modest effects
Whether lecanemab, which is administered by infusion, offers people a clinically meaningful reduction in cognitive decline has long been debated.
A phase III clinical trial of the drug, which was published1 in 2022, included 1,795 people in the early stages of Alzheimer’s disease and found that after 18 months, those who received the drug showed a 27% reduction in cognitive decline compared with those who received a placebo. Some researchers celebrated the news as a win for the field. But others argued that the effects are too small to have a meaningful effect on patients.
One reason for this difference in perspective lies in how people look at the data, says Sebastian Walsh, a public-health researcher at the University of Cambridge, UK. The 27% reduction represents the relative difference in the amount of cognitive decline experienced in the drug group versus the placebo group. The absolute difference in cognitive function is much smaller: 0.45 points on an 18-point scale. “People can extract from the effect size what they want,” says Walsh. “If they want to sell the drug, you could stick to the relative changes — and if you’re very sceptical, you could talk about the absolute differences.”
But even small effects could become meaningful if maintained over time, particularly in the later stages of the disease when decline is quicker, Walsh says. “It ultimately comes down to what you think the long-term effect is going to be, and we don’t have an answer to that.”
Some longer-term data is now available. At the Alzheimer’s Association International Conference (AAIC) in Philadelphia last month, Eisai and Biogen presented findings from an open-label extension study, which continued to monitor the patients who received lecanemab following the completion of the phase III trial. After three years of continuous treatment, more than half of patients showed improvement, and most cases of ARIA occurred in the first six months of treatment. They also reported that the rate of cognitive decline returned to placebo levels when people stopped taking the drug, even if amyloid plaques had been removed before ceasing treatment.

Lecanemab, which is sold as Leqembi, is infused into patients in a hospital every few weeks.Credit: Kota Kiriyama/Yomiuri Shimbun via AP/Alamy
Some are optimistic about these findings — Haass says that it’s exciting to see that the drug not only clears amyloid but also slows the spread of tau, another protein that accumulates into clumps in the brain of people with Alzheimer’s. Others are more cautious. Paresh Malhotra, a neurologist at Imperial College London, points out that the positive findings presented at AAIC were not compared to a placebo, so more data is needed to determine the drug’s long term effectiveness.
Cost is also a concern. Walsh says that, given the drug’s modest effects, it is difficult to justify the expense of administering the drug (which costs more the US$20,000 yearly in the United States) and the procedures, such as neuoimaging and genetic testing, that are required to identify people eligible to receive it.
Safety worries
The biggest concern about lecanemab is ARIA, which the US Food and Drug Administration (FDA) warned about in its approval. Although most cases are asymptomatic — and none were reported during the initial 18-month clinical study — there have been a handful of ARIA-linked deaths in the extended phase of the trial.
Some experts say that although the risk of severe ARIA is small, it’s also important to consider that the drug is administered during the earliest stages of Alzheimer’s. “This is the time period where people have the most to lose,” says Schrag. “We are often encouraging patients in this window to travel, to think about their bucket list, to get done the things that they want to accomplish in life.”
Ellis van Etten, a neurologist at Leiden University Medical Center in the Netherlands, says that there are still many open questions about ARIA, and how clinicians should respond when they see patients develop these abnormalities during treatment. For example: who will develop severe or life-threatening ARIA? At what point does ARIA go from being benign to harmful, and when should treatment with lecanemab be stopped?
Many of the same questions about benefits and risks apply to another amyloid-clearing antibody, donanemab — made by Eli Lilly in Indianapolis, Indiana — which received FDA approval in July. Donanemab seems to offer roughly the same degree of reduction in cognitive decline as lecanamab — and it has been associated with ARIA-related deaths.
“We know from biomarker-related work that these antibodies clear amyloid, so we know that they’re addressing a fundamental mechanism of the disease,” Malhotra says. But these drugs alone will likely not be enough, and addressing other aspects of the disease will be important, he adds. “It’s very likely that in ten years’ time, we’ll be talking about combination therapies and that amyloid-clearing will be part of this approach.”
doi: https://doi.org/10.1038/d41586-024-02720-y
This story originally appeared on: Nature - Author:Diana Kwon


















