This injectable gel can help to diagnose brain injury — then it disappears

The squishy sensors could be used to monitor the brain for tumours or injury, before eventually degrading
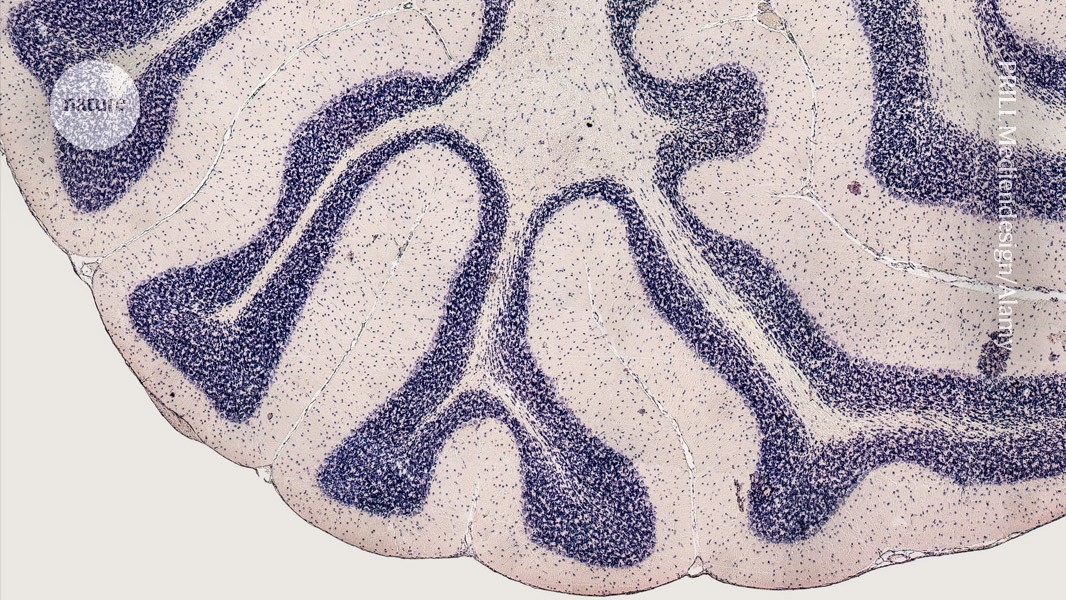
Researchers have used dissolvable sensors to monitor rat brains.Credit: PRILL Mediendesign/Alamy
Researchers have developed biodegradable, wireless sensors that can monitor changes in the brain following a head injury or cancer treatment, without invasive surgery. In rats and pigs, the soft sensors performed just as well as conventional wired sensors for up to a month after being injected under the skull.
The gel-based sensors measure key health markers, including temperature, pH and pressure. “It is quite likely this technology will be useful for people in medical settings,” says study co-author Yueying Yang, a biomedical engineer at Huazhong University of Science and Technology (HUST) in Wuhan, China. The findings were published today in Nature1.
“It’s a very comprehensive study,” says Christopher Reiche, who develops implantable microdevices at the University of Utah in Salt Lake City.
Probing the brain
For years, scientists have been developing brain sensors that can be implanted inside the skull. But many of these devices rely on wires to transmit data to clinicians. The wires are difficult to insert and remove, and create openings in the skin for viruses and bacteria to enter the body. Wireless sensors offer a solution to this problem, but are thwarted by their limited communication range and relatively large size. Developing sensors that can access and monitor the brain is “extremely difficult”, says Omid Kavehei, a biomedical engineer who specializes in neurotechnology at the University of Sydney in Australia.
To overcome these challenges, Yang and her colleagues created a set of 2-millimetre cube-shaped sensors out of hydrogel, a soft, flexible material that’s often used in tissue regeneration and drug delivery. The gel sensors change shape under different temperatures, pressures and pH conditions, and respond to vibrations caused by variations in blood flow in the brain. When the sensors are implanted under the skull and scanned with an ultrasound probe — a tool that is already used to image the human brain in clinics — these changes are detectable in the form of ultrasonic waves that pass through the skull. The tiny gel-cubes completely dissolve in saline solution after around four months, and begin to break down in the brain after five weeks.
Hot and cold
The researchers confirmed that the gel was not harmful or toxic in cell cultures. They then used a puncture needle to inject it 5 millimetres beneath the skulls of rats, and attached ultrasound probes to their heads. For comparison, they also implanted wired sensors that are currently used in clinics to track changes inside the brain.
To test the gels, the researchers first squeezed the rats’ bellies, which increased the flow of cerebrospinal fluid and blood into the brain, and induced a rise in pressure inside their skulls. The pressure-detecting sensor picked up the shift slightly more accurately than did the conventional device. It also registered the spike in pressure in the skull of a rat with a brain injury. When the team placed a heating blanket or ice pack near the rats’ heads, the temperature sensor registered the changes just as well as did the wired temperature probe.
The gel performed stably for up to a month after being injected in the brain, and then began to break down. The rats showed no signs of adverse effects by the time the sensors began dissolving. Being able to track pressure, temperature and pH could be useful for diagnosing brain injuries and monitoring them over time, says study co-author Hanchuan Tang, a biomedical engineer, also at HUST. He adds that the gel could also be implanted after the removal of tumours to monitor for cancer recurrence.
Breathing
The researchers also implanted the sensors into a pig and found that they were sensitive enough to detect minute pressure changes induced by the animal’s breathing, a feature the wired probe failed to pick up.
Although the results are impressive, more work is needed to assess whether the sensors will be safe enough to use in humans, says Julia Körner, who develops hydrogel-based biomedical sensors at Leibniz University Hannover in Germany. The big question is whether the by-products formed when the sensors break down are harmful or can accumulate in other parts of the body, she says.
Tang says they will continue to investigate the safety of their system. They also plan to fine-tune it to perform stably over longer periods, and to explore how to manufacture the devices at scale.
doi: https://doi.org/10.1038/d41586-024-01673-6
Read the related News & Views: ‘Brain fluid probed by ultrasound using squishy cubes’
This story originally appeared on: Nature - Author:Gemma Conroy


















